Surgery for Bladder Cancer
Transurethral Removal (Resection) of Bladder Tumour
This surgical procedure is used in both the diagnosis and treatment of bladder cancer. And TURBT allows Dr. Feifer to remove an entire tumor from the inside of your bladder. TURBT is a key first step to obtain a biopsy to confirm the cancer diagnosis and determine the stage and grade of your cancer. At the start of the procedure, you will be given general anesthesia or spinal anesthesia. During a TURBT, Dr. Feifer inserts a tool through the urethra to reach the bladder, which has a surgical loop on it that cuts off tumor tissue from the bladder to be assessed microscopically by the treating pathologist.
You will likely go home the same day and might be required to wear a small drainage tube called a catheter which is inserted in the penis before you wake up, to help drain your urine for a few days and allow your bladder to heal. You may experience urinary frequency or some blood in the urine after surgery which is entirely normal. Should the bleeding be significant, with blood clots, you will be required to return to the emergency room to have these blood clots evacuated. Once the pathology is ready to be discussed, we will have a discussion about what the situation is and what further treatment if any is necessary. Some patients will have intravesical therapy required, in which the chemotherapy or immunotherapy drugs are delivered directly into the bladder through a catheter to destroy any microscopic tumor cells that may still be in the bladder after TURBT. All subsequent therapy is required based on the stage and grade of your tumour will be discussed with you thoroughly, so that you fully comprehend the risks and benefits and side effects of these therapies
Radical Cystectomy and Urinary Diversion ( continent and ileal conduit)
When you have been diagnosed with muscle-invasive bladder cancer, and have been accessed via a multidisciplinary approach, one of the significant procedures that may be indicated is surgical removal of the entire bladder and tissues around the bladder, as well as reconstruction to urinate. Your kidneys clean the toxins out of your blood and make urine. Which is passed to your bladder in small muscular tubes called the ureters. When the bladder is removed, the urine coming from the ureters needs to be diverted to another area for elimination from your body. Your urethra is a tube that carries the urine out from your bladder, And may require removal as well depending on the type of cancer you have. In women, the urethra is very short. It’s located above the vagina. In men, the tube is longer. It passes through the prostate gland and penis.
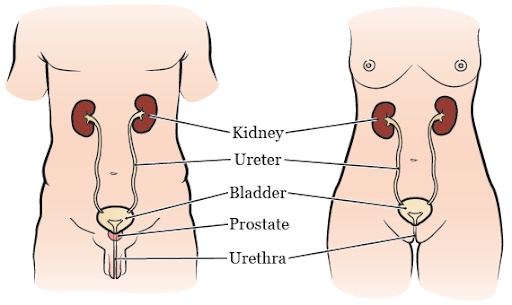
Surgery to remove your entire bladder is called a radical cystectomy. During your surgery, your nodal tissue around the bladder, which may harbour cancer cells, will be removed with your bladder. The removal of lymph nodes will not cause you any felt abnormality after surgery. If you’ve had surgery or radiation in the past, some lymph nodes may be absent or not resectable. In addition to your bladder and lymph nodes, for men, the prostate and seminal vesicles are removed, and in women, the uterus, fallopian tubes, ovaries and a part of the vagina may also be removed. A detailed assessment will be made with you before surgery, and the plan will be clear prior to the procedure.
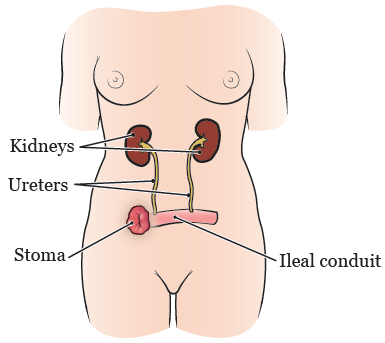
When the bladder is removed, We have to create a new passage where the urine will leave your body and this is called a urinary diversion. The type of urinary diversion that you will get depends on numerous factors. The most common is the creation of what is called an ileal conduit. during this procedure, a small piece of urine tube will be used to create a passageway where one end will open to your skin and the other end is sutured to the two ureters creating a conduit of urine through your abdominal wall which is caught in a permanent urostomy bag which you will wear on your skin on your lower abdomen. This is often the most simple urinary diversion, and allows the patient to undergo the surgery in less time and will have less maintenance in your everyday life.
The second type of diversion is called an ileal neobladder, in which a slightly longer piece of your small intestine will be used to create a new internal pouch that on one side is attached to your urethra and on the other side attached to the ureters to allow there to be an internal pouch to store the urine, similar but very different from the normal bladder. The final decision to build this complex structure will be made during your surgery, and we will talk with you about how this decision was made, add in what circumstances a backup plan would be necessary, and an Ileal conduit will be made instead. With this type of diversion, you will need to use the muscles in your abdomen and different maneuvers to empty your neobladder. After surgery, you may need to irrigate the new bladder and insert a catheter through the urethra to completely empty it. The advantage is that there was no external appliance on your abdomen, but this type of reconstruction is complex, requires a very motivated patient, and can lead to complications if not cared for very meticulously. This surgery usually takes about 4 to 7 hours.
Preparing for your surgery
We will work together with you, your family doctor, and other health professionals such as your cardiologist as appropriate to make sure that you are ready for surgery. If you had chemotherapy prior to surgery, we will work carefully with your medical oncologist to ensure that the surgery is done quickly and at the right time. There will be a thorough preoperative assessment including an evaluation of any blood thinners that you are on, any prescription medications that you are on, as well as an assessment of your medical comorbidities to ensure that all aspects of your care are taking into account before we decide to move to surgery. You also have a meeting with an anesthesiologist, to ensure that you are fully aware of the anesthetic procedure. Prior to surgery, we will ask that you refrain from drinking alcohol and not smoke. If you are a heavy alcohol user, you do not need to stop your alcohol completely, this should be discussed with the treating team.
After Surgery
After surgery, you will spend between 3 and 7 days in the hospital recovering. Motivated patients can leave very earlier. You will be managed via an enhanced recovery after surgery program (ERAS). The most critical aspect of recovery is to start moving around as soon as you can. The faster you move around, the faster your intestines will start working again, the sooner you will be able to eat, and the quicker you are able to go home and return to normal activities.
You will be encouraged to walk as much as possible to the nursing station and back to your room. After the immediate postoperative period, when you go home, you will have an orchestrated follow-up schedule explain to you, and you will see your surgeon to remove any drains or stents that may be left in place to help the healing process, and you will have a detailed assessment of your pathology with your surgeon once the microscopic analysis is completed by the Pathology Department. This final discussion regarding your surgical pathology will help dictate future risk and any other therapies that may be necessary after your surgery. Most importantly, complications such as clots in your legs, and other types of major events are possible after your surgery, so it is very important for you to stay active at home after you’re discharged from the hospital, all of these details will be discussed with you before you’re discharged. Additionally, you may be required to take blood thinning medication for a prolonged. Of time after surgery to prevent blood clots and pulmonary emboli.
Sexual Health Considerations
Bladder surgery will affect your sexual health. Your surgeon will detail all of these considerations prior to surgery, and you can attain great help at maintaining an intimate life by consulting a sexual counsellor, available to you through our office. For men, bladder surgery can cause changes in erectile function, as the nerves that control erections are very close to the prostate and bladder. This erectile dysfunction can impact your ability to maintain a normal intimate life, but it is entirely treatable, and there are many options to maintain erections after bladder surgery. As your prostate and seminal vesicles will be removed with your bladder, it will not be possible for you to father children naturally, but if fertility and family planning are important, sperm banking prior to surgery and assisted reproductive technology after surgery, including sperm extraction, it is possible for you to grow your family. For women, reproductive organs are removed at the time of bladder removal and you will not be able to bear children yourself. Women may also have changes in their sexual function after surgery. Your treating team will help you with this adaptation, to ensure that you retain a full personal life. Family planning will be discussed with you prior to surgery so that other considerations if warranted are taken into account.
TREATMENTS & CONDITIONS
Urinary Obstruction
Ureteropelvic junction (UPJ) obstruction occurs in the upper urinary. Most often, it is blocked at the renal pelvis. This is where the kidney attaches to one of the ureters

Benign Prostate Gland Enlargement (BPH)
Benign prostatic hyperplasia (BPH), also called prostate gland enlargement, is a common age associated condition. An

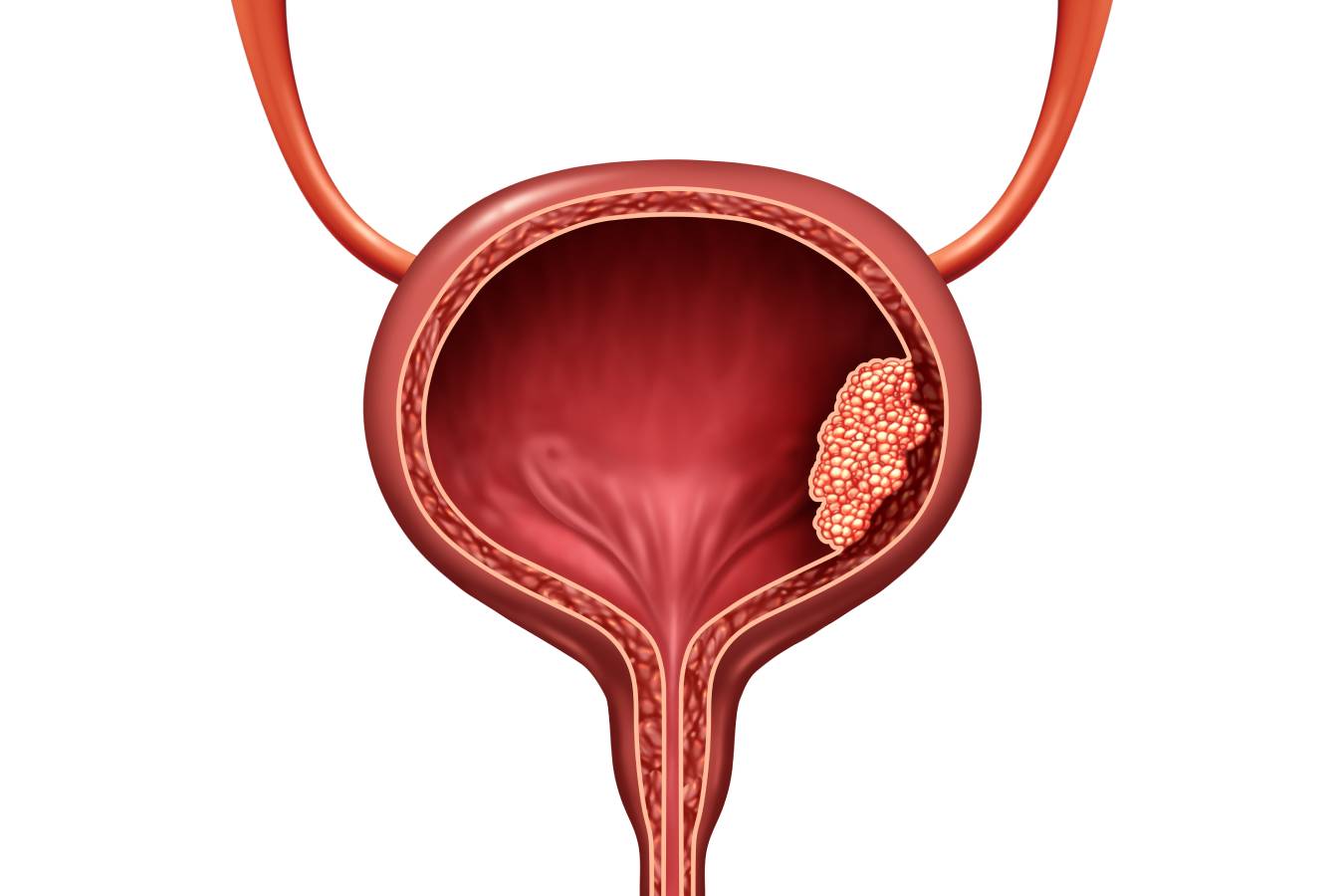
Bladder Cancer
Bladder cancer is a type of cancer that begins in the lining of the urinary bladder. The bladder is a hollow muscular organ in the pelvis that stores urine before evacuation.

Hematuria (Blood in Urine)
This is defined as blood in the urine, can be microscopic (invisible) or macroscopic (visible), and can come from anywhere in the urinary tract, from the kidneys themselves to ..


